Welcome to The Tonic, a light-hearted, heavily resourced newsletter for folks interested in learning about long COVID, ME/CFS, and other chronic illnesses. Come for the info; stay for the whimsy. Or vice versa.
I will generally post once a week on Saturdays or Sundays: a narrative post when my energy allows and resource roundups (known here as The Antidote) at all other times. Occasionally I post more than once a week, usually to announce an event or to push brief, timely info out to you sooner.
Wish list shout out!
Who doesn’t love gifts? Many of my readers have chosen to support my efforts here via the Amazon wish list in lieu of paid subscriptions (which could jeopardize my disability benefits). A big Tonic THANK YOU this week goes to wish list two-timer Jodie F.
If anyone is interested in showing support for The Tonic, see below for the info. There’s something for every budget and any help is appreciated. (Note: please be sure to include a note with your gift(s) so I can include you in the shout out!)
The Tonic is free to read - Amy is so happy you’re here! There is no paid subscription option here like with other Substack newsletters. However, if you are valuing the experience and are able, please consider a show of support by sending a gift of health, wellness, or joy from this Amazon wish list. Anyone who does gets a 📢 in an upcoming post. Thank you!
Rollin’ rollin’ rollin’
Friends, the weather has been pretty nice here in NY and I’m trying to take advantage of it before my pale, delicate, heat intolerant ass has to hibernate in the air conditioning for the bulk of the summer. Lest anyone think I’ve become this way because of Long COVID, I can assure you I was born this way.
Anyway, I’ve been enjoying taking walks outside and meeting friends for lunch/coffee/ice cream. My wallet and my waistline are taking a hit, but I’m feeling joyful and that can only help my recovery. I’ll pay off my credit cards someday. I’ll drop some of this chub eventually. Or I won’t. One of the blessings of this life-will-never-be-the-same-again brand of illness is that you gain perspective on what’s really important. If feeling healthy and strong means carrying more debt and a spare tire around my mid-section, then bring me a bigger wallet and some stretchy pants. Or any pants, really. Clearly I need some.
So here we are at part three of my recovery series, which focuses on self-care practices that have made a difference in how I feel.
For those who are new here or who may have missed them, I will link to parts one and two of the recovery series below. Part one (particularly the intro) is important to read because it lays out all of the disclaimers and qualifiers that any person with Long COVID or ME/CFS should present before claiming to have anything resembling answers to these complex chronic illnesses. In fact, I do not claim to have the answers. I only share what has been helpful and why I think this has been the case for me so you can decide if it might make a difference for you too. Much of this is the result of me reading, watching, or listening to other people’s recovery journeys and culling tools from them, so I am merely paying this forward. To quote perhaps the most important part of the intro to part one:
If you’ve met one long hauler, you’ve met one long hauler.
Try what might speak to you, leave the rest. Maybe circle back. It’s your recovery journey and you have to do what feels right.
Recovery tools, part 3
(Apologies for the terrible paragraph breaks below; nothing I did made any difference. Substack mostly has good formatting, but it’s not perfect)
Therapy
I’ve had several therapists during my four-plus years of LC, and they have all had their value. However, the one who has made the biggest difference for me is one who had her own lived experience of ME/CFS illness and recovery. You can read all about Jamie here:
I am not one of those therapy snobs who thinks it is 100% necessary for a therapist to have lived through everything I have in order to help me (how would I even find that therapist?). But navigating everyday life with an energy-depleting illness is a very unique situation that is hard for energy “normies” to fully understand. I know I wouldn’t have totally “gotten it” before, well, I got it. Jamie has personal insights into the boom-bust cycle: how singularly frustrating it is to get a little energy, overspend it, then pay for it with symptoms. She understands how my personality traits get in the way of my breaking that cycle. Jamie also gets the grief process involved in having to leave much of your former life behind and accept new realities.
Other therapists have accepted these experiences as I shared them, but so much time and energy can be saved when your therapist doesn’t need these explanations because she lived them.
Jamie is coming back from maternity leave* soon, so I’ll be starting back up with her again (yay, me!). I’m looking forward to sharing with her how much I’ve improved since we last met, which was right around when the art of pacing really began clicking for me.
*for those with LC or ME/CFS, take note: like Jamie, you can recover to the point of having that family you always wanted, or that career, or that trip, etc.).
It’s hard for me to offer this advice to folks living with LC or ME/CFS simply because they’re not easy to find, but if you can find a therapist with lived experience, I highly recommend it. And for those of you who live in NY, stay tuned: I am a licensed social worker and hope to be starting to earn hours toward my own clinical license as soon as I am able. I eventually plan to specialize in helping folks with LC, ME/CFS, and related conditions.
Sleep and non-sleep deep rest (yoga nidra, meditation, etc.)
This first one is self-explanatory, perhaps: getting as much sleep as possible has provided my body with time to heal.
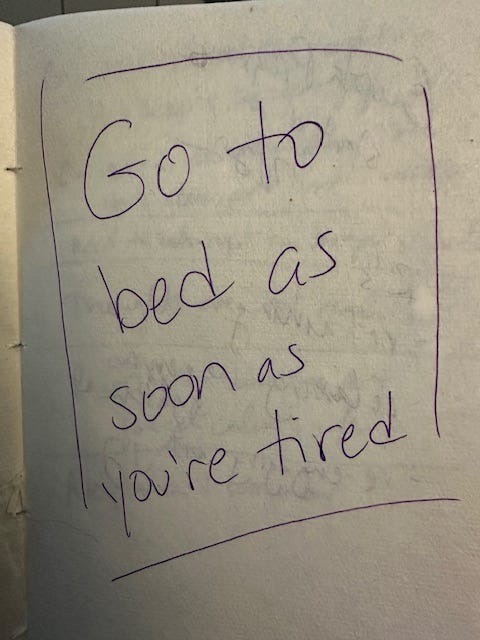
When I was still a working long hauler, I would end my workday by crashing on the couch, immobilized by the energy expenditure of back-to-back Zoom meetings, decisions, thinking, listening, and talking. I’d eventually drag my way to the kitchen to make a quick dinner or eat whatever Baldy placed in front of me. Often, I’d “rally” a small amount of energy after dinner and try to stay up to have a little bit of enjoyment in my day. We also adopted Fritzy cat in the early days of the pandemic, and I felt I owed him some play time, since I was unavailable during the day. I remember my massage therapist (who specialized in ME/CFS bodywork) at the time telling me how vital it was for me to go to bed when I was tired and not force myself to stay up longer. I wrote this in big letters on a full page of my healing journal at the time.
I realized I was letting my old patterns of thinking about squeezing every bit of life I could out of each day govern my new life, and it wasn’t working. As soon as I started following her advice, I started getting better rest.
This was not, however, enough to counteract the effects of working a stressful job while having these illnesses, and I eventually threw in the towel and took disability leave. Once I did, I allowed myself to sleep for as long as I needed to in the morning. For most of the last four years, I have gone to bed between 10:30-midnight and have awakened between 10-11am. Occasionally, I go through bouts where I naturally wake up at 8:30-9am, but right now I’m in one of the 10-11am phases. And I just go with it, because I can and my body clearly needs it. I realize this is an enormous privilege I have over those who have these illnesses and are still working or who have to wake with their children, though I do think we could all pay a bit more attention to what our bodies are trying to tell us they need and make tweaks in our daily lives when possible.
I know that many folks with LC and ME/CFS have trouble sleeping. There is often a “tired but wired” effect that happens when we feel exhausted, but our nervous systems are dysregulated and amped up. This can also become a chicken-and-egg effect with anxiety/fear and racing thoughts. I have gone through phases of this as well, especially in the first three years of the illness, when I hadn’t yet focused on regulating my nervous system. I occasionally still have nights where I just can’t fall asleep, which I suppose most people do (though in the “before times,” I rarely had trouble falling sleep).
What helps on these nights is to do a yoga nidra meditation before I try sleeping. I will sometimes do one in the afternoon also if I’ve been particularly overwhelmed. Yoga nidras are often referred to as non-sleep deep rest because they put your body in a state of extreme relaxation that can be as valuable in some cases as taking a nap. Yoga nidra is not really yoga in the sense of movement, but rather more like a meditation where you are guided to pay close attention to specific body parts, one by one. This has the effect of breaking your attention away from whatever thoughts were consuming your mind beforehand and is very soothing to the nervous system. My favorite is this one from the Insight Timer app (free):
I have also found doing 10-20 minute guided meditations to be extremely helpful in regulating my nervous system, getting me out of the sympathetic “fight-or-flight” state and into the parasympathetic “rest-and-digest” state (where we humans are meant to spend the majority of our time). There are several meditations I like on the Insight Timer app, and I also have a lifetime membership to the Calm app, where I like listening to the Daily Calm ten-minute meditations. (I do these meditations interchangeably with using my Sensate, which was discussed in part two of this series).
Gentle movement - yoga
Once I accepted the fact that I could no longer do traditional exercise or even something as simple as walking for too long, I was able to accept ‘spoonie yoga’ into my life (or as I lovingly call it, “gimp yoga”). The idea was to start with micro-movements, all done while laying down, all designed to connect the breath with movement and to ultimately teach my brain and my nervous system that movement was safe. It wasn’t going to make me worse or send me into a crash the way more ‘extreme’ movement (even chair yoga) had been doing.
For those of you who are new here, I’ve already written an entire post on this. It’s a hoot, check it out. You can also find information on how you can sign up for a free or discounted class with Nourish Therapeutic Yoga, the same gimp yoga that I take on a weekly basis:
In the next recovery post, I’ll be talking more about movement I’ve been doing lately that borders on exercise (gasp!). Stay tuned…
Breathwork
Shortness of breath was my very first symptom of acute COVID-19 and stayed with me for about 2.5 years. About six months after my initial infection, I was diagnosed with asthma after laboring to get through a pulmonary function test.
Some of you longtime Tonic readers will remember my post about mouth-taping (yes, I tape my mouth closed every night and it has been a game changer). If you are new here, check it out. I just re-read it and I humbly submit to you that it’s damn funny!
In addition to improving my breathing through mouth-taping, I also did breathwork exercises during the day that made a big difference. I read somewhere that folks with long COVID were tending to breathe very shallowly, and the goal was to learn to take slower, deeper breaths. But you can’t just start doing this and expect it to stick, since breathing is regulated by your autonomic nervous system (are you picking up on a theme here in these recovery posts? Working to calm and regulate a dysfunctional autonomic nervous system is perhaps the most important thing you can do to get your body back into homeostasis so it can attend to the tasks of healing).
In the books Breath by James Nestor (heavily cited in my mouth-taping article) and The Oxygen Advantage by Patrick McKeown, I learned the science behind the benefits of breathing well, as well as exercises one can do to improve their breathing. I also took advantage of free courses that were offered early in the pandemic by a group called Stasis, which was working in collaboration with the Mount Sinai Post-COVID Center (probably the most cutting edge of these centers in the U.S. since the beginning).
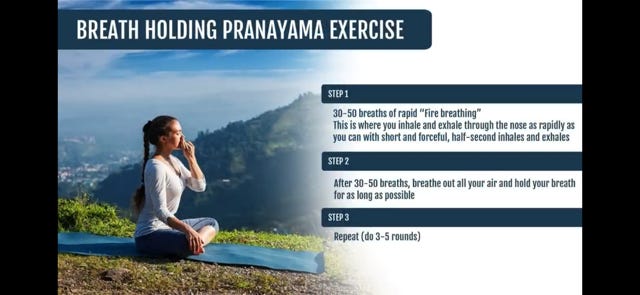
The three main exercises I did were box breathing, “fire” breathing, and the physiological sigh. Many of you will have already heard of these. Box breathing involves breathing in for a set number of seconds (usually four to start), holding that breath for the same number of seconds, breathing out for the same number of seconds, and holding again for the same number of seconds. Once you can comfortably do 4-4-4-4, you can move on to 5-5-5-5 and so on.
Fire breathing is a bit more involved and isn’t something to do when you are first starting, but it can help with the gas exchange involved with oxygen and carbon dioxide. Here’s a slide depicting how it’s done, courtesy of Ari Whitten.
The physiological sigh is a research-backed way to reduce anxiety, and it’s something we do naturally, often when we are overwhelmed or stressed. It involves taking in a long breath, followed immediately by a short breath, and ending in a long, sighing exhalation. Click on the link for a short video explaining the technique and the benefits.
I used these techniques to overcome my post-COVID asthma a few years ago. I returned to this breathwork when my shortness of breath returned inexplicably last year for a short time. They are also useful techniques for achieving a state of calm.
That’s all for this edition of Recovery tools. Stay tuned for next time when the focus is on specific practices designed to push your boundaries a bit when you are starting to get better.
Now stick around for…
🥳 The After-party 🥳
Announcements, links to articles and studies, recommendations and shout-outs, and miscellany joy and/or tomfoolery.
🦠 The annual summer wave of COVID is heading for us, folks. What should people know about the new coronavirus variant? Also, COVID rises in California as new FLiRT strains dominate.
💰 Raelan Agle interviews Dr. Eleanor Stein on Long COVID and ME/CFS recovery strategies on a budget (both Raelan and Dr. Stein recovered from ME/CFS after many years of being sick):
🖥️ Here’s the recording for the PolyBio Research Foundation Spring 2024 Symposium. PolyBio is a non-profit group dedicated to doing cutting edge research on long COVID, ME/CFS, long Lyme, and related complex chronic illnesses. This recording is five hours long, but contains short presentations by all of the researchers funded through PolyBio. It is time-stamped in the notes, so you can skip to the research that most interests you.
🍵 Yikes: Nearly 900,000 Yogi Tea Bags Recalled Over High Levels of Pesticide Residue.
💊 Here’s
with an eye-opening look at turmeric supplements:🦁 Enjoy this ferociously adorable video of animals yawning:
🤦🏽♂️ Buffoons of the week: The biggest buffoon this week? You guessed it: the whiny, farty man-child with a terrible orange combover who is now a convicted felon. But this week we have two others. Harrison Butt-ker, the Kansas City Chiefs kicker dumbass who doubled down on attacking working women and LGBTQ+ folks after his initial disgusting commentary in the college commencement speech he gave. And, this guy. In the words of the inimitable Bugs Bunny, “what a MA-ROON!”
🏆 Winners of the week: The Bay Area’s Amy Appelhans Gubser, who became the first person to swim from the mainland U.S. to the Farallon Islands, considered one of the toughest swims in the world. She’s 55 years old and the article calls her a Bay Area grandma, because get it, guys? Grandmas aren’t supposed to be able to emerge from behind their walkers and swim at the Y, let alone break world records swimming in the ocean. <non-physiological SIGH>
🐈⬛ 💩 And finally, it’s this week’s Cat Dump. Psychotic-squirrel-tries-attacking-the-shorthairs edition. (I asked my childhood bestie Danya about what could have been going on here - she is an animal expert. Her response? “That squirrel’s just an asshole” 🤣🤣🤣).

















Nice to hear about your future plans in social work, Amy, all in your own timeline. And I love the crazy squirrel at the end! I have a sort of squirrel phobia (I hate their beady eyes) so I was glad your windows seem secure! ❤️
I like “Art of Pacing”.